CCSV FAQs - Medical Theory
Synchronising the Lungs and the Heart during CPR
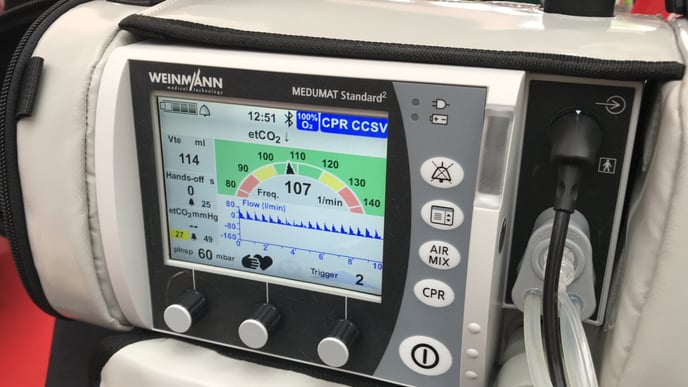
The new CCSV (Chest Compression Synchronised Ventilation) mode from WEINMANN Emergency is revolutionising ventilation during resuscitation.
CCSV is a real innovation in emergency ventilation during resuscitation. The mode can be easily integrated in the ventilator MEDUMAT Standard² from WEINMANN Emergency and also retrofitted to existing equipment.
What is CCSV?
Chest Compression Synchronised Ventilation (CCSV) is a ventilation mode that was developed exclusively for resuscitation. CCSV applies a mechanical breath synchronised simultaneously with each chest compression. With this revolutionary method, the disadvantages of conventional ventilation modes can be avoided and the gas exchange and hemodynamics improved.
The current guidelines of the European Resuscitation Council [1] recommend a respiratory rate of 10/min with pure oxygen during professional cardiopulmonary resuscitation (Advanced Life Support, ALS) after intubation by trained staff, without interrupting chest compressions. Which form of ventilator breath (manual or mechanical) and which mechanical ventilation mode should be used was, however not the subject matter of the currently applicable guideline reviews, so that no statement is made about this in the current guidelines.
Frequently, mechanical ventilation patterns are currently put into practice, such as Intermittent Positive Pressure Ventilation (IPPV) or BiLevel Ventilation (BiLevel), also during resuscitation, which were not developed for use during cyclical chest compressions. Through the small gas volumes in the ventilation system generated with chest compressions, the function of conventional ventilators can be significantly disrupted and preset volumes or pressures can no longer be correctly achieved. That is why the Chest Compression Synchronized Ventilation (CCSV) mode was developed specially and exclusively for use during resuscitation, and it demonstrates an extremely high degree of reliability in the implementation of the preset ventilation parameters. Due to the characteristic synchronisation of the mechanical breaths with the chest compressions for this ventilation pattern, it succeeds in avoiding possible negative implications of the use of conventional ventilation patterns and optimizing the gas exchange and hemodynamics at the same time. As the current guidelines of the European Resuscitation Council do not issue any recommendations in favor of a specific ventilation mode, the use of CCSV during resuscitation is not contradictory to this.
When is it suitable for CCSV and how does the mode work?
As soon as the patient is intubated endotracheally, CCSV can be used with MEDUMAT Standard² (with purchased and enabled flow measurement and CCSV software options).
The essential mechanisms can be divided into the categories hemodynamics and gas exchange. During resuscitation, special attention is given to the restoration or maintenance of perfusion, as the functioning of vital organs directly depends on it. To this end, W. Kouwenhoven et al. (1960) describe the performance of manual chest compressions, which, in unchanged form, are nowadays still an essential part of resuscitation measures [2]. Due to the compression of the chest, with the heart and lung organs inside it, a pressure gradient builds up, which causes an emission of blood. This mechanism later became known as the “heart pump mechanism”.
Chest compressions also play the key role in ventilation with CCSV. In this case, yet another principle is utilized. In 1976, Criley et al. observed that fully conscious patients who developed ventricular fibrillation under monitoring were able to maintain consciousness by simply coughing [3]. This discovery shows that a rapid increase in intrathoracic pressure can generate an arterial pressure. An increase in arterial pressure, in turn, causes an increase in cardiac and cerebral perfusion pressure. The mechanism described is also referred to as the “chest pump mechanism” and, on closer examination, can also be observed during ventilation with CCSV.
In this case, the rapid increase in intrathoracic pressure due to the delivery of the mechanical breath synchronously with the chest compressions causes a higher arterial pressure in comparison to IPPV and BiLevel. In summary, a higher cardial and cerebral perfusion pressure and an improved organ perfusion are accordingly assumed during resuscitation with CCSV ventilation.
In the case of gas exchange, CCSV causes an improved oxygenation of the blood. Furthermore, both a normal decarboxylation of the blood and a normal pH value are observed. In several animal experiments, the arterial oxygen partial pressure (PaO2) was significantly higher than under IPPV or BiLevel [5] [6].
Has CCSV already been examined in studies?
Yes. To date, a total of four studies have examined the use of the CCSV ventilation pattern. Three studies were conducted in a pig model and another was conducted in a specially developed simulation model.
Data from animal experiments (pig model):
- Study 1: IPPV/BiLevel/CCSV (n=24): Exploratory study of feasibility and safety [4]
- Study 2: IPPV-CCSV crossover (n=12): Examination of 3 CCSV settings regarding gas exchange and hemodynamics [5]
- Study 3 IPPV-CCSV group comparison (n=44): Gas exchange, hemodynamics, cerebral oxygenation, ROSC, post-resuscitation phase, histology [6]
Data from Simulation model:
- Study 4 IPPV/BiLevel/CCSV (n = 90 paramedic): feasibility of preset ventilation parameters [7]
How does the device detect chest compressions and in which phase are mechanical breaths delivered?
A defined low expiratory gas flow, as typically occurs at the start of each chest compression on intubated patients, is the trigger for the beginning of inspiration. The sensitivity of the trigger can be manually adjusted by the user. In this way, any necessary adaptation to particular lung characteristics is made possible.
In the novel ventilation mode CCSV, the mechanical breaths are applied simultaneously with the automatically or manually performed chest compressions. The ventilation frequency is thus identical with the compression frequency (100-120/min). Consequently, very short inspiratory times (Tinsp = 205 ms) are necessary. In order to achieve an inspiratory gas flow in spite of the simultaneous chest compressions and the positive effect on the hemodynamics described above, comparatively high inspiratory pressures of up to 60 mbar are necessary (cf. Figure 1). As a result, depending on the condition of the lungs, tidal volumes of 100 ml to 200 ml are achieved.
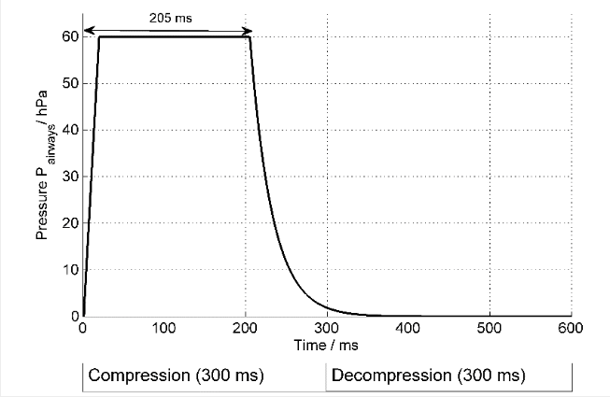
Figure: How Chest Compression Synchronized Ventilation (CCSV) works: Ventilation is pressure-controlled with Pinsp = 60 mbar during the compression phase of the chest compression (Tinsp = 205 ms). No ventilation takes place during the decompression phase.
Relatively high ventilation pressures arise during resuscitation. Are these harmful to the patient?
High airway pressures (> 40 mbar) regularly and frequently occur during conventional ventilation under resuscitation due to the ventilation performed asynchronously to the chest compressions. Under certain circumstances, these pressures can even far exceed 60 mbar. The setting of an inspiratory pressure limit with conventional IPPV ventilation, for example, does not usually prevent these pressure peaks, as particularly at the end of the inspiratory phase, the administered tidal volume is already in the lung and is not able to escape with the very fast pressure increase at the beginning of the chest compression. This can lead to uncontrolled pressure peaks during ventilation. In CCSV mode, the maximum airway pressures are limited to 60 mbar due to the synchronous, pressure-controlled ventilation. Furthermore, ventilation is only carried out with small tidal volumes of approx. 2 ml/kg body weight (bw). The volume load of the lungs in terms of volutrauma is therefore lower than during conventional ventilation with up to 7 ml/kg ideal body weight (IBW) and simultaneous chest compressions. Furthermore, no macroscopic or histological lung damage was observed during the use of CCSV in the animal model. [6]
In the studies in the pig model [6, 4, 5, 7] with a total of more than 70 test animals, after a total of 30 minutes of resuscitation, no macroscopic or histological lung damage was observed that could be attributed to the use of CCSV or differed from the results for IPPV ventilation.
Another reason for this assumption is the fact that during the use of CCSV the delivery of the mechanical breath is synchronized with the compression phase of the chest compression, and consequently a defined pressure always arises in the lungs. When conventional ventilation patterns are used, asynchronous insufflation can cause a lung already filled with air to be compressed by the chest compression. In comparison to CCSV, this can even cause higher intrapulmonary pressures and potentially increase the likelihood of lung damage.
The Guidelines say that hyperventilation is to be avoided. Isn't that exactly what CCSV does?
The recommendation to avoid hyperventilation is based on two hypotheses:
1. Hyperventilation during resuscitation causes a higher intrathoracic pressure during the decompression phase. This can reduce the venous return flow to the heart. Consequently, the cardial and cerebral perfusion pressure may fall.
2. Hyperventilation produces hypocapnia, which, in turn, can have negative impacts on both the arterial pressure and cerebral perfusion.
During ventilation with CCSV, the intrathoracic pressure increases exclusively during the chest compression and not during the decompression phase, when venous return flow occurs. The feared effect of a perfusion reduction therefore does not occur. In fact, Total perfusion is even improved.
Furthermore, the calculated respiratory minute volume under CCSV actually significantly exceeds the known physiological values. Nevertheless, the effective alveolar ventilation volume is largely identical to IPPV ventilation with a tidal volume of 7 ml/kg KG and a ventilation frequency of 10/min, after deducting the dead space ventilation. This is also confirmed by experimental data, which document a normocapnia under CCSV. [6]
Is there a risk that CCSV results in only dead space being ventilated?
The results of studies so far show that the applied respiratory minute volume leads to improved oxygenation and normocapnia and the measured tidal volume was always above the dead space volume. [6] [5]
Consequently, it can be assumed that CCSV results in adequate and even improved alveolar gas exchange and not only dead space being ventilated.
Can CCSV be used on children and/or infants?
Are high PaO₂ values detrimental if the SpO₂ is already 100%?
During resuscitation, a high PaO2 is preferably aimed for, as even with the best possible chest compression, the cardiac output and the tissue perfusion, particularly of the brain, are lowered significantly. Even with optimized ventilation, as with CCSV and a FiO2 of 1.0, during resuscitation, only normal or slightly increase tissue oxygen saturation values are measured in the brain tissue, so that there is no risk of hyperoxia. When the spontaneous circulation returns (return of spontaneous circulation, ROSC), however, the value of the tissue oxygen saturation in the brain already rise significantly in the early reperfusion phase, which is why after ROSC, with securely measure SpO2 values, a SpO2 of above 98% should be avoided.
Is PEEP detrimental and does it lead to a reduced venous return?
With CCSV, only low PEEP values are applied of below 5 mbar, so that no negative influencing of the venous return occurs. Due to the exceptionally good oxygenation under CCSV, in principle, no PEEP is required, however, in several cases, such as with prolonged resuscitation or in pulmonary edema, for example, a low PEEP improves the trigger behavior with CCSV by increasing the functional residual capacity.
Was the DO₂ measured during the study?
In one of the animal experimental studies, the avDO2 was measured immediately after ROSC, which showed a significantly higher avDO2, i.e. a higher oxygen extraction in the IPPV group compared to CCSV with similar cardiac output. This can be interpreted as an oxygen deficit, which occurred during the previous resuscitation.
Is CCSV suitable for use with supraglottic airway aids?
Even with increased airway pressures, CCSV requires an impermeable, secured airway, in order to develop its full effect. For this reason, it is only recommended to regularly use CCSV in connection with endotracheal intubation or a blocked larynx tube.
CCSV has a ventilation frequency of 100/min. How can the CO₂ be effectively exhaled during the short expiratory time of CCSV?
CCSV operates with a high ventilation frequency and low tidal volume, however, these are greater than the pure dead space volume. This creates an effective alveolar respiratory minute volume that is similar to the values of IPPV. This is sufficient for eliminating enough CO2.
References
FAQs written by WEINMANN Medical Technology
[1] Soar, Jasmeet; Böttiger, Bernd W.; Carli, Pierre; Couper, Keith; Deakin, Charles D.; Djärv, Therese et al. (2021): European Resuscitation Council guidelines 2021: Adult advanced life support. In: Resuscitation 161, p. 115–151. DOI: 10.1016/j.resuscitation.2021.02.010.
[2] JUDE JR, KOUWENHOVEN WB, KNICKERBOCKER GG. (1960): Clinical and experimental application of a new treatment for cardiac arrest. In: Surg Forum.1960;11:252-4.
[3] J. Michael Criley, Arnold H. Blaufuss, Gary L. Kissel (1976): Cough-Induced Cardiac Compression Self-administered Form of Cardiopulmonary Resuscitation. In: JAMA. 1976;236(11):1246-1250. doi:10.1001/jama.1976.03270120022018
[6] Dersch, Wolfgang; Wallot, Pascal; Hahn, Oliver; Sauerbrei, Christopher; Jerrentrup, Andreas; Neuhaus, Christian et al. (2012): Resuscitation and mechanical ventilation with Chest Compression Synchronized Ventilation (CCSV) or Intermitted Positive Pressure Ventilation (IPPV). Influence on gas exchange and return of spontaneous circulation in a pig model Category: CPR Systems. In: Resuscitation 83, e3. DOI: 10.1016/j.resuscitation.2012.08.010.
[4] Kill, Clemens; Hahn, Oliver; Dietz, Florian; Neuhaus, Christian; Schwarz, Stefan; et al. (2014): Mechanical Ventilation During Cardiopulmonary Resuscitation With Intermittent Positive-Pressure Ventilation, Bilevel Ventilation, or Chest Compression Synchronized Ventilation in a Pig Model. In: Critical Care Medicine: February 2014 - Volume 42 - Issue 2 - p e89–e95. doi: 10.1097/CCM.0b013e3182a63fa0
[5] Kill, Clemens; Galbas, Monika; Neuhaus, Christian; Hahn, Oliver; Wallot, Pascal; Kesper, Karl et al. (2015): Chest Compression Synchronized Ventilation versus Intermitted Positive Pressure Ventilation during Cardiopulmonary Resuscitation in a Pig Model. In: PloS one 10 (5), e0127759. DOI: 10.1371/journal.pone.0127759.
[7] Speer, T., Dersch, W., Kleine, B. et al. Adv Ther (2017) In:34:2333. doi.org/10.1007/s12325-017-0615-7
[8] Evans, Elen; Biro, Peter; Bedforth, Nigel (2007): Jet ventilation. In: Continuing Education in Anaesthesia, Critical Care & Pain 7 (1), S. 2–5. DOI: 10.1093/bjaceaccp/mkl061.
[9] Chang, H. K. (1984): Mechanisms of gas transport during ventilation by high-frequency oscillation. In: Journal of Applied Physiology 56 (3), S. 553–563. Available online at http://jap.physiology.org/content/56/3/553.