CCSV FAQs - Practise, Application & Troubleshooting
The CCSV ventilation mode can be easily integrated in the resuscitation process and is compatible with manual chest compression, as well as with automatic cardiopulmonary resuscitation devices.
How is CCSV switched on in the device?
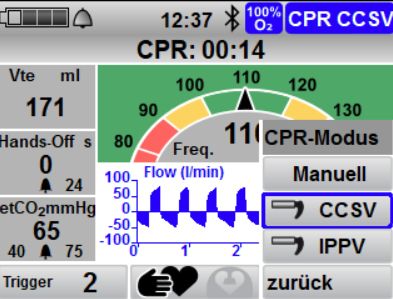
By pressing the CPR button on the device, the user enters the resuscitation mode set by the operator. Depending on the pre-setting, CCSV mode must still be selected from the submenu. In MEDUMAT Standard², resuscitation mode (CPR mode) has the following structure:
In the absence of chest compressions, the device automatically switches from CCSV mode to IPPV mode as back-up ventilation after a defined period of between 10 and 60 seconds and returns to CCSV when compressions begin again.
What is the effect of setting the trigger?
The triggers enables the user to change the sensitivity in detecting chest compressions. This can be set within a range from 1 to 5. With trigger level 1, the device reacts most sensitively to the chest compressions performed, while level 5 is the least sensitive setting.
No mechanical breaths are delivered in CCSV ventilation mode despite chest compressions – what should I do?
- Make sure that you are in CCSV ventilation mode and that all components are connected correctly.
- Reduce the trigger level – as low as trigger level 1.
- If mechanical breaths are still not applied, increase the PEEP.
- If compressions are still not detected, switch to CPR-IPPV mode.
Why is a PEEP required under CCSV?
The preset PEEP of 3 mbar under CCSV is used to increase the intrathoracic volume. This is especially necessary at the start of CCSV in order to generate an adequate volume flow from the lungs by means of the compressions and, consequently, an adequate trigger signal.
An increase in the functional residual capacity (FRC) by means of a moderate PEEP is useful under CCSV to ensure an adequate trigger function. This is especially the case if the FRC is reduced considerably due to obesity, significant secretion, pulmonary edema or after aspiration. Negative impacts of a moderate PEEP are unlikely under CCSV, as an intrinsic PEEP of up to 10 mbar is inherently reached during CCSV ventilation.
Consecutive mechanical breaths are delivered in CCSV ventilation mode without chest compressions – what should I do?
If mechanical breaths are delivered in CCSV ventilation mode without chest compressions being performed, mechanical breaths may have been wrongly triggered (autotrigger). In this case, increase the trigger level (less sensitive), e.g. from 2 to 3.
In CCSV ventilation mode, only every second chest compression is followed by a mechanical breath – what should I do?
Due to the defined very low inspiratory time of approx. 200 ms and a subsequent minimum expiratory time, a correct triggering is only possible up to a maximum chest compression frequency of 140/min. If compressions are performed more frequently, only every second chest compression can be detected and synchronized. For this reason, make sure that the maximum chest compression frequency does not exceed 120/min in line with the guidelines.
Hyperventilation is suspected under CCSV – what should I do?
Under CCSV, the tidal volumes are typically approx. 2 ml/kg (IBW). Should the tidal volumes measured by MEDUMAT Standard² significantly exceed this (> 200 ml), reduce the Pinsp from 60 mbar to 40 mbar.
What happens if MEDUMAT Standard² does not detect chest compressions despite the trigger setting being corrected?
If you are in CCSV resuscitation mode and the device does not detect chest compressions, the device automatically switches to back-up ventilation (IPPV) and ventilation is carried out as usual.
What happens if chest compressions are no longer performed due to ROSC?
As soon as chest compressions are no longer detected, MEDUMAT Standard² switches to IPPV back-up ventilation. As soon as MEDUMAT Standard² detects chest compressions when resuscitation becomes necessary again, the device automatically returns to CCSV mode with an inspiratory oxygen concentration of 100 % – even if the oxygen concentration has been previously manually reduced after ROSC.
Can mechanical resuscitation devices also be used with CCSV?
Yes, compatibility with Corpuls CPR, and other mechanical chest compression devices (AUTOPULSE & LUCAS) has been verified. If a mechanical chest compression device is used, the setting on the device must be changed from manual chest compression to mechanical chest compression. The frequency tachometer is then gray and the frequency alarms are deactivated.

During the use of CCSV with a mechanical resuscitation device, the “Frequency high” alarm appears – what should I do?
Make sure that “mechanical chest compression” is set under CCSV. Should the alarm persist, increase the trigger level, e.g. from 3 to 4.
Why does the device have to be switched from manual to mechanical resuscitation or vice-versa?
Switching is necessary, as the triggers in “mechanical” mode are optimized for mech. chest compression. In this way, an improved detection of chest compressions is possible. Furthermore, the compression frequency alarms are deactivated in the mechanical mode.
The patient has aspirated. Is it possible to use CCSV?
Yes, in principle, it can be used. Aspirate the airways as usual and then use CCSV. In the absence of mechanical breaths, reduce the trigger level, so that it is more sensitive, and consider raising the PEEP.
The CO₂ (etCO₂) value measured at the end of exhalation is relatively low, but all other measurement pa-rameters are within the standard range – why?
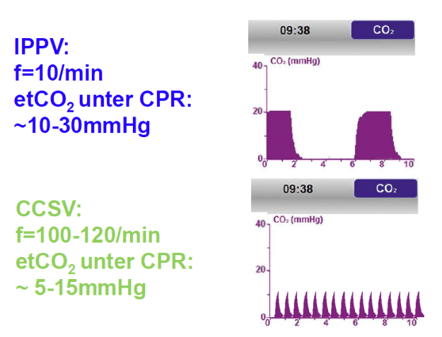
In principle, normocapnic values are achieved by the use of CCSV. [6] As the mechanical breaths are administered with a comparably high frequency and a mixture of exhalation gas and fresh gas is only created by low tidal volumes in the ventilation system in the area of the measurement gas suction or measuring cuvette, the etCO2 measured value of the ventilator or defibrillator is usually lower than with conventional ventilation under resuscitation (see figure). Consequently, the value should not be used as a prognostic value.
The return of spontaneous circulation (ROSC) during chest compression and CCSV ventilation causes a significant relative rise in etCO2, just like during conventional ventilation. A clear assessment of the actual paCO2 under CCSV(as is also the case with conventional ventilation under resuscitation) can only be provided by a blood gas analysis (BGA).
The patient has a very stiff lung or fluid in the lungs – how should CCSV be set in this case?
Aspirate the airways as usual and then use CCSV. In the absence of mechanical breaths, reduce the trigger level, so that it is more sensitive, and consider raising the PEEP.
The device shows lines as a CO₂ measured value, what should be done?
Check the CO2 on MEDUMAT Standard² during the analysis phase of the defibrillator. During this phase, complete expiration occurs and the device can measure the CO2value.
References
FAQs written by WEINMANN Emergency Medical Technology
[1] Soar, Jasmeet; Böttiger, Bernd W.; Carli, Pierre; Couper, Keith; Deakin, Charles D.; Djärv, Therese et al. (2021): European Resuscitation Council guidelines 2021: Adult advanced life support. In: Resuscitation 161, p. 115–151. DOI: 10.1016/j.resuscitation.2021.02.010.
[2] JUDE JR, KOUWENHOVEN WB, KNICKERBOCKER GG. (1960): Clinical and experimental application of a new treatment for cardiac arrest. In: Surg Forum.1960;11:252-4.
[3] J. Michael Criley, Arnold H. Blaufuss, Gary L. Kissel (1976): Cough-Induced Cardiac Compression Self-administered Form of Cardiopulmonary Resuscitation. In: JAMA. 1976;236(11):1246-1250. doi:10.1001/jama.1976.03270120022018
[6] Dersch, Wolfgang; Wallot, Pascal; Hahn, Oliver; Sauerbrei, Christopher; Jerrentrup, Andreas; Neuhaus, Christian et al. (2012): Resuscitation and mechanical ventilation with Chest Compression Synchronized Ventilation (CCSV) or Intermitted Positive Pressure Ventilation (IPPV). Influence on gas exchange and return of spontaneous circulation in a pig model Category: CPR Systems. In: Resuscitation 83, e3. DOI: 10.1016/j.resuscitation.2012.08.010.
[4] Kill, Clemens; Hahn, Oliver; Dietz, Florian; Neuhaus, Christian; Schwarz, Stefan; et al. (2014): Mechanical Ventilation During Cardiopulmonary Resuscitation With Intermittent Positive-Pressure Ventilation, Bilevel Ventilation, or Chest Compression Synchronized Ventilation in a Pig Model. In: Critical Care Medicine: February 2014 - Volume 42 - Issue 2 - p e89–e95. doi: 10.1097/CCM.0b013e3182a63fa0
[5] Kill, Clemens; Galbas, Monika; Neuhaus, Christian; Hahn, Oliver; Wallot, Pascal; Kesper, Karl et al. (2015): Chest Compression Synchronized Ventilation versus Intermitted Positive Pressure Ventilation during Cardiopulmonary Resuscitation in a Pig Model. In: PloS one 10 (5), e0127759. DOI: 10.1371/journal.pone.0127759.
[7] Speer, T., Dersch, W., Kleine, B. et al. Adv Ther (2017) In:34:2333. doi.org/10.1007/s12325-017-0615-7
[8] Evans, Elen; Biro, Peter; Bedforth, Nigel (2007): Jet ventilation. In: Continuing Education in Anaesthesia, Critical Care & Pain 7 (1), S. 2–5. DOI: 10.1093/bjaceaccp/mkl061.
[9] Chang, H. K. (1984): Mechanisms of gas transport during ventilation by high-frequency oscillation. In: Journal of Applied Physiology 56 (3), S. 553–563. Available online at http://jap.physiology.org/content/56/3/553.